How do I protect my spouses assets from Medicaid?
Table of Contents
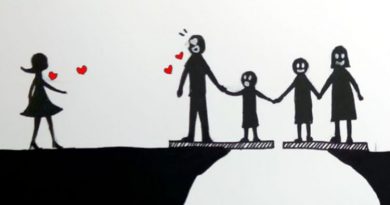
How do I protect my spouses assets from Medicaid?
Create a Funeral Trust – Certain irrevocable funeral trusts created for the Medicaid candidate and / or their spouse can enable a couple to reduce their countable assets by up to $30,000 (depending on their state of residence).
Is spouse turning 65 a qualifying event?
Once someone reaches age 65, active enrollment in Medicare must occur by applying for this Social Security benefit. Although a loss of coverage occurs when employees voluntarily remove themselves from the health plans, the reason (attaining other coverage, including Medicare) is not considered a qualifying event.
Can one spouse get Medicaid and the other not?
Medicaid assumes that both spouses of a married couple are financially responsible for one another. As a result, when Medicaid determines a spouse’s eligibility for benefits, the assets of the husband or wife who isn’t applying — known as “the community spouse” — are expected to contribute to the care of the other.
Can a spouse elect Cobra without the employee?
Each qualified beneficiary has a separate right to elect COBRA continuation coverage. For example, the employee’s spouse may elect continuation coverage even if the employee does not. COBRA continuation coverage may be elected for only one, several, or all dependent children who are qualified beneficiaries.
Can Cobra coverage spouse only?
COBRA requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain specific events.
Can you be denied Cobra coverage?
Under COBRA, a person who has been terminated for gross misconduct may be denied COBRA. The former employee may not be in any position to elect continuation coverage or pay the COBRA premiums. However, he or she may have a spouse or dependents who qualify to continue to live in the United States.
Can I get cobra if I’m fired?
Under COBRA, you usually can keep your health-care coverage after you leave your job, even if you were fired.
How much is Cobra health insurance per month?
With COBRA insurance, you’re on the hook for the whole thing. That means you could be paying average monthly premiums of $569 to continue your individual coverage or $1,595 for family coverage—maybe more!
Does Cobra coverage begin immediately?
Assuming one pays all required premiums, COBRA coverage starts on the date of the qualifying event, and the length of the period of COBRA coverage will depend on the type of qualifying event which caused the qualified beneficiary to lose group health plan coverage.
Is Cobra cheaper than Obamacare?
The cost of COBRA insurance depends on the health insurance plan you had under your employer. COBRA costs an average of $599 per month. An Obamacare plan of similar quality costs $462 per month—but 94% of people on HealthSherpa qualify for government subsidies, bringing the average cost down to $48 per month.
How do I calculate Cobra costs?
Locate the amount you contribute on your pay stub. Locate the amount your employer pays in the insurance enrollment paperwork or call the employer’s human resources department. Add the amount you contribute each month to the amount paid by your employer. Multiply the total monthly cost by the percentage you will pay.
How long does an employer have to send out Cobra information?
Your business has 90 days to provide the employee with a COBRA General Notice, which basically describes the employee’s rights and obligations under COBRA. When a qualifying event occurs. Your business must notify the employee of their COBRA rights within 14 days of the qualifying event with an election notice.
Can I cancel Cobra and get a refund?
Generally, there are no refunds. You can contact your administrator or your past employer for specific insurance payment information.
When can you terminate Cobra for non payment?
There’s a minimum 30-day grace period for late premium payments, so the plan cannot terminate your coverage if, for example, you’re 10 days late in paying your premium one month. 5 But if you don’t make your premium payment either on time or within the 30-day grace period, your coverage can be canceled permanently.
When can Cobra be terminated?
When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums. Coverage under another plan.
Can you cancel Cobra and get Obamacare?
Losing or canceling your COBRA doesn’t disqualify you from getting an ACA subsidy, but it may impact your eligibility to enroll in an individual market plan. 1 You can enroll in a Marketplace (exchange) plan and apply for a subsidy during this special enrollment period.
Is Cobra cheaper than private health insurance?
COBRA may still be less expensive than other individual health coverage plans. It is important to compare it to coverage the former employee might be eligible for under the Affordable Care Act, especially if they qualify for a subsidy. The employer’s human resources department can provide precise details of the cost.
Can I get covered California instead of Cobra?
Most consumers will pick either COBRA or Covered California, but some may need to pick both to avoid a gap in coverage. If you enroll in a Covered California plan and make a payment before your employer coverage ends, Covered California will pick up where your employer coverage leaves off. There is no need for COBRA.
What if the cobra is better than the new Employers Insurance Can I keep the cobra?
You may continue COBRA for up to 18 months as long as you do not obtain other insurance or become covered under your new employer’s group health policy. You can not have COBRA continuation and another insurance at the same time.
Do you lose benefits when laid off?
If you’re laid off: For employees who are terminated, benefits usually end with your job and you’ll have to pay for health insurance yourself. Plus, if your employer has gone out of business, the health plan is usually terminated, so COBRA won’t be available.
Do you lose insurance when laid off?
Losing health insurance coverage — no matter if you were laid off, let go with cause, you quit or any other reason — qualifies you to apply through Covered California 60 days before and after the date your coverage stops. This period is called special enrollment.
Who pays for Cobra after termination?
1. Must I pay for a terminated employee’s COBRA coverage? No. An employer can require an electing employee to pay up to 102% of the cost of the medical coverage in order to continue coverage under COBRA.
Can you buy Cobra for 2 weeks?
If, in those 45 days, you secure other coverage either through your new employer or somewhere else and you didn’t have any health care claims, you simply don’t pay your COBRA premium. It means you didn’t really have COBRA, but you had the option available.
What if my employer does not offer me cobra?
Generally, when an employer fails to offer COBRA coverage, it must send the election notice and offer the coverage retroactively. However, if the offer is extremely late – meaning the maximum coverage period has ended – the employer may offer coverage going forward.