Can I stay on my husbands health insurance after divorce?
Table of Contents
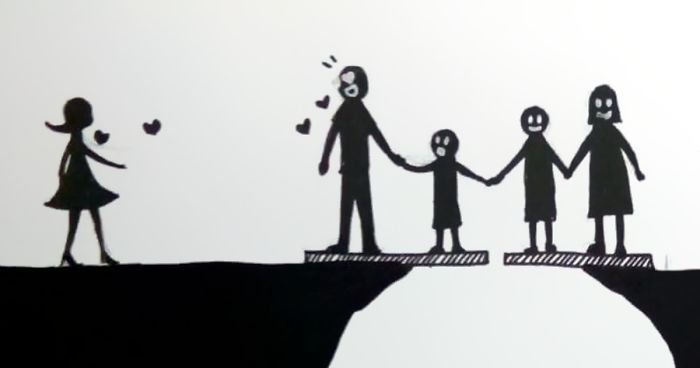
Can I stay on my husbands health insurance after divorce?
After you get divorced, you may be able to temporarily keep your health coverage through a law known as “COBRA.” If your former spouse got insurance through an employer that has at least 20 employees, COBRA lets you stay on that plan for up to 36 months.
Can I drop my wife from health insurance?
Once you are married and on your spouse’s insurance, you cannot remove them from your insurance policy prior to a divorce. However, if you read the reasons why the law exists, it states that a spouse cannot be removed from health insurance prior to a divorce. Then the law will start to make more sense.
Which parent is responsible for health insurance?
The parent who claims the children on his or her income tax return as dependents is the one required to provide proof of health insurance with the return. Impact: It is generally the custodial parent who claims the children as dependents and the non-custodial parent who is required to pay for the health insurance.
Do I have to provide health insurance to my ex wife?
While your children will continue to receive coverage, your ex-spouse will likely not meet the requirements. That said, the Consolidated Omnibus Budget Reconciliation Act (COBRA) requires employers to keep providing health insurance for an employee’s ex-spouse for up to 36 months after a divorce.
Is it OK to have 2 health insurances?
Splitting your health insurance between two providers can sometimes provide better value premiums or coverage than taking out combined hospital and extras cover.
How is primary and secondary insurance determined?
If you have coverage under a plan from your employer in addition to a spouse’s or parent’s plan, your own plan will be primary and the other plan will be secondary. This is also true if the additional coverage is with TRICARE or Medicaid, as those plans are always the secondary insurer if you have other coverage.
How does dual insurance coverage work?
Dual insurance occurs where two or more insurance policies cover the same insured risk. Claims for dual insurance between insurers are often complicated by ‘other insurance’ clauses whereby a policy seeks to exclude or limit coverage because of the existence of the other policy.
How does primary and secondary dental insurance work?
The plans set forth rules to determine which plan pays first, (“primary”) and which plan pays afterwards (“secondary”). The general rule is that the plan that covers you as an enrollee is the primary plan and the plan which covers you as a dependent is the secondary plan.
Do you still pay a copay if you have 2 insurances?
Normally patients that come in with 2 insurances should not be charged a copay. In most cases their secondary policy will pick up the copay left from the primary insurance. We recommend you bill those particular patients after both insurances process the claim for any remaining copay.
What is the point of secondary insurance?
Secondary health insurance is coverage you can buy separately from a medical plan. It helps cover you for care and services that your primary medical plan may not. This secondary insurance could be a vision plan, dental plan, or an accidental injury plan, to name a few.
Do you have to pay your co pay at the ER?
Next time you go to an emergency room, be prepared for this: If your problem isn’t urgent, you may have to pay upfront. While the uninsured pay upfront fees as high as $350, depending on the hospital, those with insurance pay their normal co-payment and deductible upfront.
Why is my insurance copay so high?
Why so high? Typically when you have a health insurance plan with a low monthly premium (the monthly payment), you’ll have a higher deductible. This means you won’t be paying a lot for your monthly bill, but if you need to use your insurance, you’ll have to pay for medical expenses until you reach your deductible.
Is it better to have a copay or deductible?
Copays are a fixed fee you pay when you receive covered care like an office visit or pick up prescription drugs. A deductible is the amount of money you must pay out-of-pocket toward covered benefits before your health insurance company starts paying. In most cases your copay will not go toward your deductible.
What does it mean when you have a $1000 deductible?
If you have a $1,000 deductible on any type of insurance, that means you must spend at least that amount out-of-pocket before your insurance company begins to pick up some of the tab. Practically all types of insurance contain deductibles, although amounts vary.
Do copays go toward deductible?
In most cases, copays do not count toward the deductible. When you have low to medium healthcare expenses, you’ll want to consider this because you could spend thousands of dollars on doctor visits and prescriptions and not be any closer to meeting your deductible. 4. Better benefits for copay plans mean higher costs.
What is out of pocket vs deductible?
Essentially, a deductible is the cost a policyholder pays on health care before the insurance plan starts covering any expenses, whereas an out-of-pocket maximum is the amount a policyholder must spend on eligible healthcare expenses through copays, coinsurance, or deductibles before the insurance starts covering all …
What happens when you meet your deductible and out of pocket?
In other words, before you’ve met your plan’s deductible, you pay 100% for covered medical costs. In contrast, your out-of-pocket limit is the maximum amount you’ll pay for covered medical care, and costs like deductibles, copayments, and coinsurance all go towards reaching it.